“My Voice” by Jamie Lynn McClelland
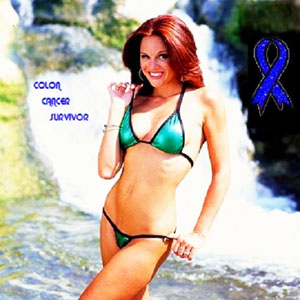
Jamie Lynn McClelland - 'Survivor'
My story begins in 1982, when I was 6 years old. That is when I lost my mother to Colon Cancer. In 1982, there was no talk of Colon Cancer being hereditary.
Fast forward 18 years. In January 2000 I consulted with my primary care physician about the loose stool I had been having. He ran some labs and even knowing my mother’s history, told me I had Irritable Bowel Syndrome. I asked him if I needed to do a colonoscopy and he said not until I turned 30.
In March of 2000 I started with a new therapist. As we began talking during the first session about the death of my mother, the therapist asked me when my last colonoscopy was, to which I replied that the doctor told me I didn’t need one until I was 30. She was shocked. She proceeds to walk over to her rolodex and get the number to her gastroenterologist, all the while telling me how she is in remission from hereditary colon cancer. Before I leave her office that day she has me make an appointment with her GI. Little did I know she was saving my life?
In May 2000 I met with Dr. Robert Just, my GI. He ran some labs and came to the conclusion that he saw no signs that pointed to colon cancer but that just to be safe, given my mother’s history, we would do a colonoscopy. On May 15th, 2000 my life was forever altered. My GI, came in after the scope and was completely speechless. He had never seen anything like it. At 23 years old my colon was covered in fields of polyps from one end to the other. He said there was no way around surgery my colon would have to come out. A few days later I had a genetic test done that confirmed I had FAP, Familial Adenmotous Polyposis. FAP is caused by a mutation in the APC Gene.
On June 22, 2000 I had a Total Colectomy and a polypectomy in my small intestine. After surgery, my colorectal surgeon estimated I would have had two years left on my life, had I not had the surgery. At 25 I would have been dead. I wouldn’t have even made it to my primary care physician’s recommendation of having a colonoscopy at 30. I was lucky. Only one polyp had spread outside the colon wall but they were able to remove all of it. My lymph nodes came back clean. There would be no need for chemo or radiation. I spent nine very long days in the hospital before heading home.
Everything seemed to go pretty smoothly. I had endoscopies every 3 months for the first year, every 6 months for the next 3 years and then went to yearly endoscopies. I had bowel slowdowns a few times that required a few days in the hospital but overall I coasted through.
In June 2004, during my annual endoscopy, Dr. Just discovered a very large polyp in the duodenum of my small intestine. He felt it was too large for him to take out so he sent me to see Dr. Isaac Raijman in Houston. Dr. Raijman is one of the top GI doctors in the country. In August 2004 Dr. Raijman performed a polypectomy and found no signs of cancer. I had a follow-up endoscopy with him in February 2005 where he found everything to be normal. He felt I could go back to my annual endoscopies with no problem.
Two uneventful years go by. During a routine endoscopy with a new GI, Dr. Stephen Utts, he discovers a very large polyp on my duodenum, again. He recommends that the polyp be removed in thirds during an endoscopy every two weeks. He also gives me a new diagnosis, Gardner’s Syndrome. Gardner’s Syndrome is a sister disease of FAP. It affects 1 in 1 million. It is caused by the same gene mutation but has other symptoms such as abnormal jaw bone structure and polyps in the small intestine. Once again, just as fate would have it, I was seen at the same time by a new oral surgeon. Upon looking at my x-rays and medical history, he confirmed, I indeed had Gardner’s Syndrome. FYI – I am certified 1 in 1 million 😉
Over the course of the next six weeks I have endoscopies to remove the large polyp. All my pathology comes back clean. After the third endoscopy Dr. Utts says he will see me in three months.
In July 2007 I have my three month endoscopy check-up. Dr. Utts tells me the large polyp is back and I should consider contacting Dr. Raijman in Houston. That’s it. Feeling uneasy about the situation and the lack of communication with Dr. Utts, I schedule an office visit with him. Finally, in September 2007, I nail Dr. Utts down about the severity of my case. He tells me that if the polyp isn’t taken out all at one time it runs a high risk of turning into cancer. I leave his office and immediately schedule an office visit with Dr. Raijman in Houston.
In October 2007, my husband and I travel down to Houston. After reviewing Dr. Utts notes, Dr. Raijman says there are two options, both required surgery. On one hand there was a relatively minor surgery where a surgical team would go in and cut a window in the small intestine and remove the polyp. I would be kept in the hospital for a couple of days for observation and then sent home. On the other hand was a major surgery, the Whipple Procedure. The Whipple Procedure is a long, invasive surgery in which your gallbladder, duodenum, part of the bile duct and part of the pancreas are removed. Dr. Raijman said he could not make a definite decision on which procedure would be necessary until he did an endoscopy himself.
On November 6th, 2007 I checked into St. Luke’s Hospital in Houston, Texas. Dr. Raijman did an endoscopy that day and 15 minutes later he knew that the only choice was to do the Whipple Procedure. Part of me was devastated and part of me was relieved. In discussions with my husband prior to this trip to Houston I had decided that a Whipple Procedure would be the best operation for long term health. I figured since it removed the entire duodenum, which seemed to be the only area that plagued me with polyps, I would have a greater chance at not having to have surgery again. Then there was the part of me that was frightened at the thought of having major surgery again.
On November 7th, 2007 I underwent the Whipple Procedure. My surgical team did an amazing job. However, there was a problem. Even with the nasal gastric tube, I was still vomiting and dry heaving. For about a week I couldn’t even keep water down. Finally, on November 15th, my surgical team did another surgery to cure my case of Pancreatitis. After that it was smooth sailing. Finally on November 23rd, after 17 days in the hospital I was able to go home.
The road to recovery once I got home was littered with pot holes. As soon as I got home I developed a fever that lasted about a week. Thank you, pancreatitis. I was also still getting sick about once a day, 5 to 7 days a week. It was beyond rough at times. In the year after the Whipple I spent 7 days back at St. Luke’s in Houston because I was throwing up pretty routinely (February 14 – 21, 2008); 10 days at Seton Austin March – April 2008 because my digestive system (or what is left of it) wasn’t breaking down food; and yet another surgery to remove a very large piece of scar tissue (yes, another sort of major surgery) in September 2008 and 10 days in the hospital.
The word “survivor” means so many things to me. Being a survivor strengthens my cancer advocacy voice. Being a survivor fuels a fire inside of me to live every day to the utmost. Being a survivor makes me savor every moment. Being a survivor means never having to say I’m sorry for being passionate about ANYTHING. However, at the same time being a survivor, I’d be lying if I didn’t admit it, I live every day in fear that the monster will return.
At the end of the day I still feel blessed. I’m alive. The month before my Whipple Procedure I was chosen as Mrs. March in the Hot Cancer Survivors 2009 bikini calendar. I hope this March to bring a younger face to Colon Cancer. It is so important to me to get the message out there that Colon Cancer is not just an over 40 disease. While Gardner’s Syndrome affects a small percentage of people (1 in 1 million), FAP affects 1 in 8000, usually before the age of 25.